On the evening of 15 March 2022, Lucille and Dave Strachan had supper in their north Wales home, watched their favourite TV show, Dogs Behaving (Very) Badly, then went upstairs to bed. Apart from one bout of food poisoning in the 1970s, Dave had never been ill before. But at about 11.20pm he woke up and told Lucille he had chest pains and difficulty breathing.
Lucille called their daughter Hilary, a doctor, before dialling 999 and asking for an ambulance. Was Dave breathing, the call operator asked. Yes, but he has chest pains and he’s cold, said Lucille. The call operator asked her to monitor Dave, to tell them every time he took a breath, information which was then fed into a computer.
Lucille was told the ambulance would take about four hours to arrive. “I thought: ‘I’m not going to wait four hours!’” she says. “So I rang my 86-year-old neighbour, Gareth the farmer.” It was past midnight now, but Gareth came immediately with his son Tudor and daughter-in-law Nia. If they could just get Dave downstairs and into the car, thought Lucille, she could drive him to hospital herself. But looking at the steep stairs inside and the slate steps and darkness outside, while considering Dave’s height – 6ft 2in – they decided they couldn’t manage. They would wait.
The neighbours stayed and Tudor headed into the lane outside with a torch so the ambulance could see which way to come. When he saw blue lights flashing in the valley below he thought: “Here it is.” But the ambulance carried on along the valley road to the nearby nursing home. “Then it left without the blue lights going, which didn’t make sense,” says Lucille. “It obviously wasn’t transporting a person, otherwise they would have had the lights on the way back as well.”
Lucille kept phoning the emergency services about the ambulance. At about 4.30am – almost five hours after she had first called – she sent the neighbours home. There was nothing much they could do and they had work the next day. She waited alone with Dave for a few more hours, while he drifted in and out of consciousness, rambling about physics. “I didn’t understand what he was saying, except when he said he was cold and I put some more blankets on him.”
She and Dave had been together for 52 years and were both 76. After Dave retired from his job as an engineer for Shell and Lucille from hers as a French teacher, they would get in their motorhome every year and head off to Italy for holidays. They loved their motorhome. Lucille remembers one evening when they were both reading in bed: “I had my motorhome magazine and there was this letter from a man who was 90 and still driving his. I said to Dave: ‘Do you think that’ll be us, will we still be doing that when we’re 90?’ And he said: ‘Well, I jolly well hope so.’”
Dave would have been reading something more intellectual than a motorhome magazine, Lucille says. “He loved anything to do with history, and mysticism, but also crime stories.” And computing; Dave built his own computers.
 View image in fullscreen
View image in fullscreen
Just before 7am, after a wait of more than seven hours, an ambulance finally pulled up to the gate. “I thought: ‘Thank God.’” says Lucille. Their decorator Paul, who had turned up earlier, rushed out and told the two paramedics to hurry because Dave was really ill. “But before the two men got out of the ambulance, another call came in and they said: ‘We’ve got to go.’ I said: ‘What do you mean, you’ve got to go?’ They said: ‘Because we haven’t put our foot out of the cab, we have to obey orders and go to another case.’ I said: ‘Dave is really ill.’ They were embarrassed. One of them said: ‘I’m so sorry, this is a red call.’ I said, ‘What’s a red call?’ He said, ‘It’s when they’ve stopped breathing.’ I said to him: ‘I’m sorry I didn’t lie and say Dave had stopped breathing.’ They turned the ambulance around and drove off.”
Lucille didn’t know about the colour codes in Wales for prioritising cases. “Because there was such a backup of cases and ambulances, Dave had been triaged down from red to amber.” Red denotes an immediately life-threatening situation. In those cases, they try to reach the patient within eight minutes. Amber is still life-threatening or serious, but there’s no target response time in Wales apart from “as soon as we can”.
The wait continued. Paul drove to Manchester to pick up the Strachans’ other daughter, Fiona. Hilary was getting a lift to their home. Because the house is on a steep hill, the valley below is visible, and some time later Lucille was relieved to see another ambulance starting up the road to them. Then that one turned back too.
“They decided it was the wrong hill,” she says, “it was too steep.” It is a steep hill, although not too steep for the previous ambulance, or for the Strachan’s motorhome, for Tesco deliveries, or for the ambulance when it eventually made it up. But first it went off down the A5 towards Corwen, then doubled back and into Llangollen, and then it was driven up an old drover’s road, which really is too steep. The people in the ambulance were lost, probably because they weren’t local, they’d come from the other side of the Berwyn mountains. (Although at this point I’m going to say I travelled from London and got to the house no trouble, I just went where my phone told me to.)
Eventually, at 9.10am, nine hours and 52 minutes after Lucille’s first call, the ambulance arrived. The two paramedics went upstairs, assessed Dave, said he was very ill, and got him down in a wheelchair. They told Lucille they would take him to Glan Clwyd – which is not the nearest hospital, but has a coronary care unit. Then they asked her for directions. Lucille wanted to go with them, but they said no. She thinks perhaps they thought they might have to perform CPR on Dave during the journey.
Dave had an oxygen mask on and had come round. He gave Lucille a thumbs up and a big smile. “I thought: ‘Oh good. It’s going to be all right.’”
It is no secret the NHS is facing huge, even existential challenges. Lord Darzi’s report, published in September, found it to be in a critical condition and hardly a day goes by without a headline containing words such as crisis and broken. See also: underfunding, underinvestment, staff shortages, burn out, outdated buildings, computer problems, cancellations and backlogs. Plus, an awful lot of waiting. Waiting for GP appointments, waiting on the phone, waiting for mental health care, waiting in A&E, waiting to get in to hospital, waiting to get out of hospital, waiting to get on a waiting list. The latest Referral to Treatment (RTT) figures, just for England, show a waiting list of 7.64m cases, made up of 6.33 million individual patients. Of those, 3.19 million people have been waiting for more than 18 weeks and 282,700 have been waiting for more than a year.
A lot of people, like Dave, have had to wait for an ambulance. One patient in Wales waited 46 hours and 46 minutes after a fall. Ambulance response times vary across the UK. In England they rose sharply in September, and emergency care performance is also down, as the NHS heads into a difficult winter. A Guardian investigation found that, in 2022, the year Dave Strachan spent nine hours and 52 minutes waiting for an ambulance, more than 500 patients in England died after a delayed ambulance response. This included people who had been in accidents, and victims of strokes and heart attacks.
In August, the head of the ambulance service in Wales said the number of hours lost because crews were waiting to hand over patients had quadrupled since 2018. Handovers – the time it takes for a patient arriving by ambulance to be handed into the care of A&E staff – are regarded as a key indicator of a system under pressure, according to the Nuffield Trust, as delays occur “as a result of a mismatch between A&E/hospital capacity and the number of elective or emergency patients arriving.” An A&E full to bursting causes queues – and a lack of social care means people have to stay in hospital beds even when they might be physically well enough to go home. Not unlike coronary circulation itself, it is all interconnected; a decrease in flow or a blockage here leads to failure or arrest there.
Some time after Dave was driven away, Lucille and her daughters Fiona and Hilary – who had now reached their parents’ home – got a call from the hospital. They were told that Dave had arrived, was being looked after and that they should wait. Half an hour later, another call. Lucille needed to come immediately. “I knew straight away it was too late.”
Paul drove them the 35 miles over the Horseshoe Pass to Glan Clwyd hospital. “The doctor,” says Lucille, “Dr Das, he was amazing. He took us into a side room and explained …”
 View image in fullscreen
View image in fullscreen
Fiona is sitting with us today, and she helps her mum out, taking over. “He said they’d tried to stabilise him so that they could operate, but he was struggling to breathe, he was just too ill. So he said he’d given him some morphine to make him comfortable and held his hand as he passed over. He was such a nice man, it’s comforting to know Dad was with someone so kind.”
Dave died of acute myocardial infarction and coronary artery atheroma. A heart attack in lay terms, although that doesn’t tell the whole story. At the inquest last year, the coroner concluded that, “The time it took for an ambulance to be dispatched and arrive and convey him to hospital meant that there was a missed opportunity to have probable life-saving medical treatment.” In other words, he probably should be alive today. Fiona says Dr Das seemed frustrated when he gave evidence at the inquest, saying if Dave had got to hospital within two hours, “there’s every chance he would still be here”.
After Dave’s inquest, the coroner wrote a Report to Prevent Future Deaths, copies of which were sent to both the Welsh Ambulance NHS Trust and the Betsi Cadwaladr University Health Board, which provides NHS services in north Wales. The report highlighted areas of concern and two reasons for the delay were given.
First was that, “All available resources were managing incidents of a higher acuity or the same category but registered prior.” Red calls, in other words, or amber calls that were made before Lucille first dialled 999. Lucille questions the whole process of calls being categorised and prioritised. “You’re asking a traumatised wife with no medical training to talk to a medically unqualified call handler with a computer algorithm and a script, and that decides whether he lives or dies. That’s basically it, isn’t it?”
The other reason why it took so long for Dave’s ambulance to come, wrote the coroner, was that “there were significant handover delays across all Betsi Cadwaladr University Health Board sites.” If an ambulance crew is unable to hand over a patient at the hospital, it can’t go and pick up the next one. “Deaths are occurring and will continue to occur as a result of delayed ambulance attendances caused by these multifactorial issues.”
The NHS is in the blood of Lucille’s family. One daughter is a hospital consultant; Lucille’s mother was a district nurse in Wales, with stories of battling across snowy moors to deliver babies. An uncle was a mental health nurse. “I still think of the NHS as one of our treasures,” she says, “one of the jewels in the crown in our country.”
Does she feel differently about it since Dave’s death? “I still think it’s a wonderful system. In this country, you have the luxury of knowing that your illness will be looked after and you won’t be made bankrupt, you won’t have to sell your house. In the US, it’s very different.”
Lucille makes it clear she doesn’t blame anybody personally. At the end of the inquest, one of the paramedics spoke to her. “A junior ambulance lady, who hadn’t been there for very long, came over and said: ‘I want to apologise, I’ve been having sleepless nights about this.’ I said: ‘Well, you can stop that right now, Dave would not want that.’”
Nor does she blame anyone at the hospital Dave was taken to. “There was a highly trained specialist waiting in an operating theatre, and the theatre staff, all waiting for him, but he couldn’t get there. It’s the system and the organisation that’s at fault.” She criticises people who go to A&E when it’s unnecessary. “It’s accident and emergency, not you’ve had a little bit too much to drink, come and clog up the system.” Plus the lack of social care places. “There are too many people in hospital who don’t need to be there.” Responding to the coroner in north Wales, the health board reported that, at the time of Dave’s death, a third of its beds were occupied by people waiting to be discharged from hospital.
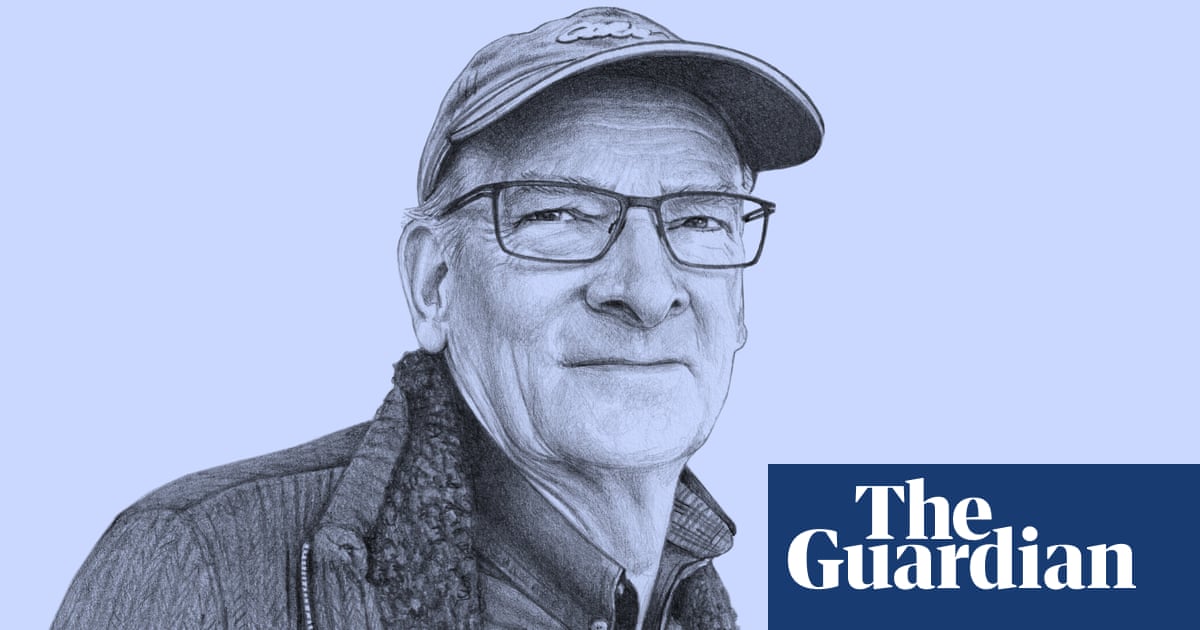
Lucille shows me pictures of Dave. He is wearing a cap and looking mischievous. Dave could never be serious for photos. “He was very witty, cheerful, respected and … yeah, loved by everybody. I sound boring, don’t I? But he was just a lovely man, my other half.” After Dave died, Lucille felt “numb for about a year” and she still hasn’t got used to life without him. “It feels as if he’s on a business trip, and he’s going to come through the door at any minute and say: ‘I’m back.’”
Fiona is helping her pack up the house, so she can move into a smaller place down in Llangollen. Lucille says the motorhome has already gone. “I don’t want to go on my own.”
∎